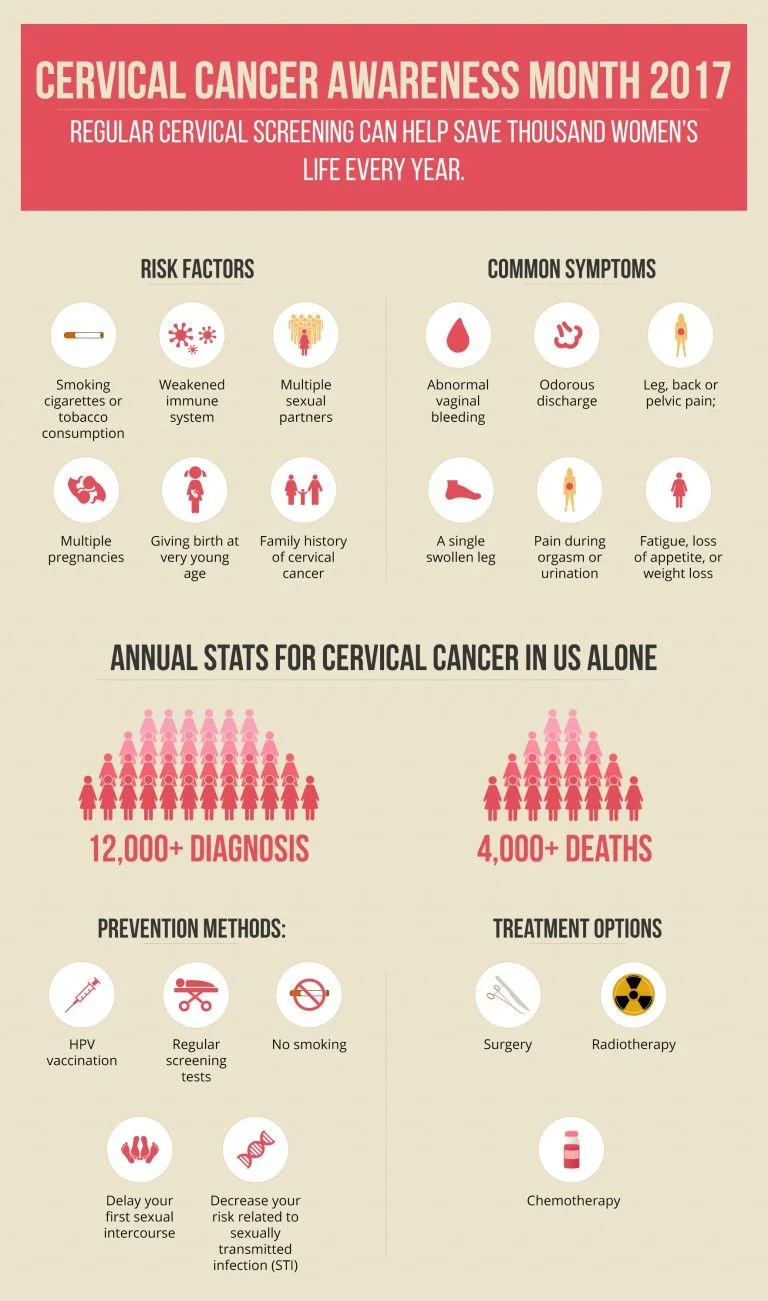
January is the Cervical Cancer Awareness Month which is a great chance to raise awareness regarding how women can improve their safety and protection from HPV and cervical cancer. According to the estimation made by Cancer.net:
There was a time when cervical cancer was one of the most common causes of deaths of American women due to cancer. However, over the past three decades, the cervical cancer death rate has shrunk by more than 50%. Increased use of screening tests is the main reason behind all this change. Screening can help you find changes in the cervix before any infection, leading to cancer, develops. It can also diagnose cervical cancer in its early stages - when it's tiny, has not yet spread, and is easier to cure. Having your children vaccinated against HPV (human papillomavirus) is another way to help them avoid cervical cancer in the future.
In most of the cases, HPV is the primary cause of cervical cancer, along with being responsible for many other kinds of cancers, too.
Let's Build a Healthy Community initiative by Pulse Uniform encourages you to consider these necessary steps and to put them into your action:
Of all the types of cancers, cervical cancer is the second most common disease affecting women worldwide. Cervical cancer originates from a woman's cervix - the lower, narrow portion of the uterus, connecting the vagina and uterus. Since it is slow-growing health disorder, it can be treated if diagnosed in its early stages. However, cervical cancer symptoms may not appear; therefore, regular preventive screenings are required. According to a recent estimation published online on Cancer.net, nearly 13,000 new cases of cervical cancer are diagnosed annually, and more than 4,000 women die due to the disease every year in the United States alone. Another study published on RHO.org suggests that about half a million women are diagnosed with cervical cancer, and more than 270,000 victims of the fatal disease die from it worldwide annually. It is mostly caused by a common virus infection, viz. Human Papillomavirus (HPV) that rapidly spreads through sexual activity.
Cervical cancer is caused by severe abnormal variations within the cells of the cervix. Since such cells normally undergo constant change, most of the precancerous or cancerous cells' changes occur in the cervix during transformation zone. In this natural process of variations, if you are infected with high-risk types of Human Papillomavirus (HPV), some cervical cells can become extremely abnormal. Other factors contributing to the development of the cancer may include:
Cervical cancer symptoms are often noticed only when it has already reached an advanced stage. As the cancer grows, the patient may experience one or more of the symptoms mentioned below:
If cervical cancer is diagnosed, the stage of the disease matters a lot in choosing the right treatment. Your doctor will conduct several tests to ascertain the stage of your cancer that informs the health expert how fast it has spread. Staging defines the extent of the health issue that is used as follows:
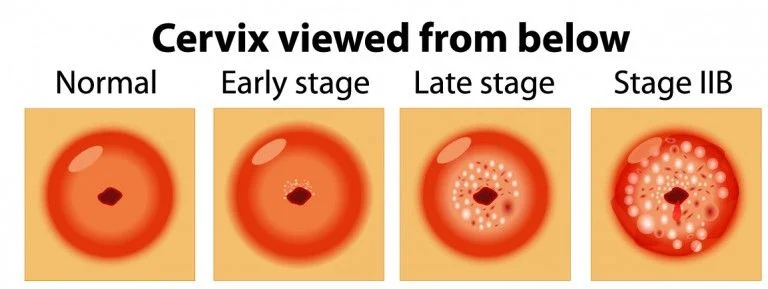
Carcinoma in situ (CIS) explains that there are cancerous changes with some of the cells of the cervix. However, the abnormal cells are limited to the surface layer of the cervix. Though CIS is not cancer, in some females the changes may develop into cancer after few years. It can be noticed during cervical screening tests. It is essential to have treatment for CIS as soon as possible. As long as the affected portion is removed, cervical cancer can successfully be prevented.
The tumor has crossed the cervix beneath the top layer of cells. And cancer cells are noticed only in the cervix; however, cervical cancer symptoms are hardly noticed.
The tumor reaches the upper part of the vagina or extends beyond the cervix into the surrounding tissues towards the pelvic wall. However, it has not yet grown in the lower third of the vagina or into the ligaments or muscles of the pelvic wall.
Spreading away from the cervix and extending to the upper part of the vagina, the tumor may have grown into the pelvic muscles and ligaments and down into the lower part of the vagina. It may also have crossed the pelvic wall. Moreover, if the tumor inhibits the flow of urine, one or both kidneys may have been affected.
In this advanced stage of cervical cancer, the cancer extends the cervix and womb, spreading to other organs of the body, like the rectum or bladder or beyond both.
Cervical cancer can successfully be prevented if changes in the cervix are found earlier before getting developed into cancer and treated if it is diagnosed in its infancy. Consequently, regular cervical screening can help save thousand women's life every year. That is why the American College of Obstetricians and Gynecologists recommends women aged 30 years or over that they should take a PAP test as well while having the HPV test.
The American Cancer Society estimates that in U.S. over 11,000 women are diagnosed with invasive cervical cancer, and about 4,000 die due to it each year. Experts believe that majority of the deaths can be prevented if all woman undergo cervical screening as recommended. According to U.S. authorities, a female should start having a screening test within three years of her first sexual intercourse or at the age of 21 - whichever occurs first. The screening does not detect any cancer; it merely looks for abnormal variations in the cervix cells. If such changes are detected and left untreated, some abnormal cells can develop into cancer after some time.
This test is designed to determine if the patient is infected with any types of HPV viruses that are most likely to cause cervical cancer. It involves collecting cells from the woman's cervix for lab testing. The test can help detect high-risk HPV strains in DNA of the cell before any cervix cell abnormalities appear.
If cervical cancer is suspected or the PAP test has revealed some abnormal cells, the patient might be required to undergo additional tests. The other tests, such as CT Scan, MTI, and Pelvic Ultrasound, may also include:
A tiny section of infected tissue is taken under common anesthetic practice to further examine under a microscope.
The doctor may perform a colposcopy, a painless examination, to detect the cervix for abnormal areas. He or she uses a colposcope, which is a special lighted instrument that magnifies the cells of the vagina and cervix, to have a better examination for superior results.
The specialist may take a mini cone-shaped section of infected or abnormal tissue from the cervix to examine if it exhibits any cervical cancer signs.
It allows the physician to scrutinize the cervix and vagina more thoroughly.
Using magnetic fields, an MRI produces exhaustive images of the body to measure the tumor's size.
While the sufferer is under anesthetic, the surgeon may recheck the pelvic area to find if the cancer has extended to any organ surrounding the cervix, such as uterus, vagina, rectum, or bladder.
The test is conducted to measure the number of blood cells and identify any kidney or liver issues.
A cancer specialist or expert health professional may be better able to tailor treatments for cervical cancer to different patients considering the cervical cancer signs and staging as discussed earlier. However, other factors may also affect their treatment options such as the type of the cancer (adenocarcinoma or squamous cell), exact spot of the cancer within the cervix, how quickly it is growing, their age and overall health, and whether they wish to conceive children in future. Treatment for early stage cervical cancer which is limited to the cervix has a good success rate. As the cancer spreads, the success rate gets lowered.

Mostly surgery is applied when the cancer is confined to the cervix. However, radiotherapy may also be utilized to reduce the risk of recurrence or if the specialist believes there may still be some cancer cells inside the body. Moreover, the patient may also receive chemotherapy if the doctor wants to lessen the tumor to make it convenient to operate; however, such practice is not very common.
When the cancer has invaded the cervix and spread beyond thereof, surgery may not be an effective option because it has become invasive which requires more extensive treatment. Consequently, the patient will typically undergo either radiotherapy or a combination of chemotherapy and radiotherapy. A palliative therapy is administered in the later stages of the disease to relieve the cervical cancer symptoms and improve the quality of life.
Participating in a clinical trial can prove to be the best treatment option for some patients which is an integral part of the cancer research process as well, contributing to cancer research and innovation. Several current treatments are the success results of clinical trials that are carried out to know the effectiveness of new treatments and ensure if these are better and safer than existing ones.
By reducing risk factors causing cervical cancer, you can treat early cervical cell variations (dysplasia). You can also mitigate your risk for abnormal cell changes. Mentioned below are some prevention methods for a cervical cancer:
Since most of the cervical cancers are caused due to HPV, having your children vaccinated against HPV, cervical cancer rates will be decreased substantially.
Regular cervical screening makes it much more likely that the signs of changes in the cervix are picked up early and tackled with before cancer develops at or too far. Your recommended Pap test schedule depends on your age and other factors increasing your risk. Consult your doctor regarding how often you need this test.
Women who consume tobacco or smoke cigarettes are at a higher risk for changes in cervical cells leading to cervical cancer. Quitting smoking may reduce such risk.
Decrease your risk related to sexually transmitted infection (STI)It is easier to prevent an STI, including HPV, than treating an infection once it occurs. Moreover, symptoms of HPV infection are barely noticed; consequently, you or your sexual partner may not know if infected by it. To reduce your risk:
Inquire about STIs, before having intercourse, with your partner if he or she is infected with it. Certain STIs, like HIV, can take up to six months before these are noticed.
Be responsible and avoid sexual contact:
The lesser the number of sex partners you have during your life span, the safer you are from an STI.
Use condoms to reduce STI risks. Furthermore, it prevents the risks of multiple pregnancies which also one of the factors triggering the disease.
Delay your first sexual intercourseStudies suggest that females having sexual intercourse during their early teens or before are at higher risk of developing cervical cancer. Therefore, delay your first sexual intercourse. Moreover, it helps you avoid being pregnant at a very young age which is another factor contributing the risks of the disease.